Hypothesis does not mean it is a fact. It means based on certain observations, it may be worth while to collect data, conduct experiments and tests, analyze them and see if they answer any pieces of the puzzle (scientific question).
Hypothesis: a supposition or proposed explanation made on the basis of limited evidence as a starting point for further investigation.
Hypothesis 1: Are a significant number of COVID deaths due to aggressive ventilatory intervention (mechanical ventilation, supplementary oxygen etc)? If so to what extent?
1. Comparing COVID deaths in Mumbai slums vs New York.
Summary:
- In spite of Mumbai slums being one of the poorest and one of the densest populated parts of the world, the number of deaths in Mumbai slums are extremely low particularly when compared to New York, another densely populated area.
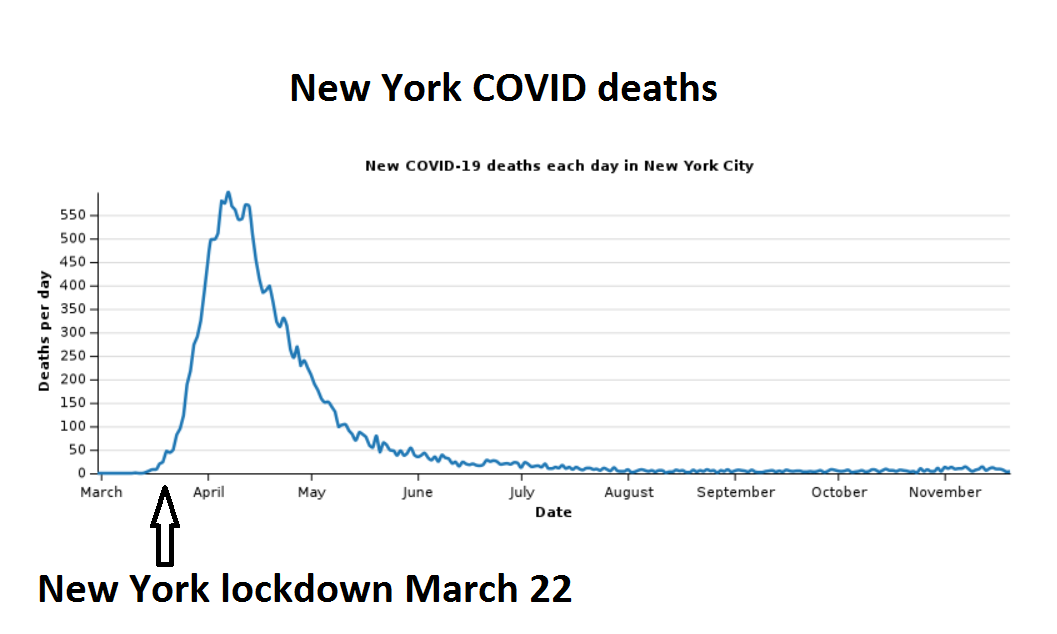
- Although the lock downs in both the Mumbai slums area and New York are comparable, the number of deaths in New York peaked after the New York March 22nd lock down.
- Mumbai slums do not come anywhere close to the level of access of medical equipment and treatment options that are available in New York.
The inconsistencies in the number of deaths in different parts of the world makes you take a look at what worked and what did not work.
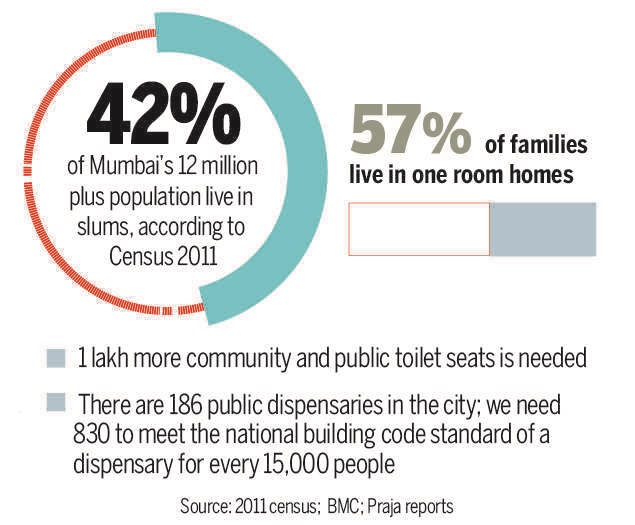
One of the largest slums in Mumbai – Dharavi, in the heart of Mumbai, India’s financial and entertainment capital, has an area of over 520 acres and a population of more than a million people. With a population density of over 277,136/km2 (717,780/mi2), Dharavi is one of the most densely populated and one of the poorest areas in the world. The population density in Dharavi slums is more than 10 times that of Manhattan.
COVID in Mumbai Slums
A Mumbai slums study published in the Journal of Urban Health December 2020, found that although a large section of people had been infected with COVID, many people survived with no or little symptoms, leading to a low mortality rate in this area.
Around 80% of people in the Mumbai slums depend on community toilets, and eight to ten people live in households or hutments just 10 × 10 ft. In this study the population was checked and re-checked with thermal scanners and oximeters. Anyone with symptoms would be sent for lab tests and quarantined. Within a few weeks, municipal teams had completed the gargantuan task of screening 548,270 people in Dharavi, including thousands of senior citizens, who are more vulnerable to the infection. According to the study, the suspected cases were shifted to well-organized COVID care centers and quarantine centers. All contacts staying in slum settlements and using community toilets were considered high risk and shifted to quarantine facilities. The study attributes the low mortality in Dharavi to timely screening, early isolation and continuous monitoring.
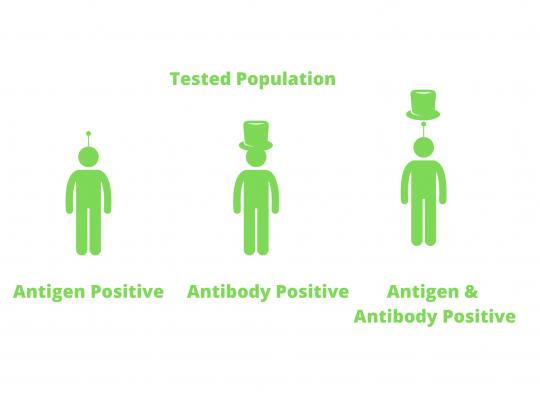
A survey carried out by Mumbai city’s municipality, a government think-tank Niti Aayog and the Tata Institute of Fundamental Research, found that 57% of the people tested in the Mumbai slum areas of Chembur, Matunga and Dahisar had been exposed to COVID by July 2020.
To understand how high the infection rate was in Mumbai slums (57% tested antibody positive), compare this to only 16% of people living outside Mumbai slums in the same areas were found to be exposed to the infection. The results were from random testing of some 7,000 people in three densely-packed areas in early July. In addition, compare this to only 16.6% London residents in May, 20% New York City residents in July, and 14% Stockholm residents in May, reportedly tested positive for antibodies.
The high prevalence rate in the Mumbai slums expectedly could partly be explained by the fact that residents share common facilities such as toilets. “The results showed how crowding plays a key role in the spread of the infection,” Dr. Juneja said. The study also found that a large section of people had been infected and survived with no or little symptoms, leading to a low fatality rate in these areas – one in 1,000 to one in 2,000.
“This is very interesting. We do not know the reason. It could be anything from social behaviour to underlying physiological differences,” Dr. Kolthur said.
Source: India coronavirus: ‘More than half of Mumbai slum-dwellers had Covid-19’
While the study attributes the Mumbai slums’ success to “chase the virus” model, in an area where 57% of the people share 1 room homes and the majority of whom use public shared toilets when compared to better living conditions such as in New York, it is difficult to explain why the deaths in the Mumbai slums have not increased after the reversal of lockdown (as of December 2020).
In another Mumbai slums study : Seroprevalence of SARS-CoV-2 in slums versus non-slums in Mumbai, India, the data showed that 54·1% of samples in slums and 16·1% of those in non-slums tested positive in July —a significant difference (p<0·001).
This study says “combined with reported COVID-19 cases and numbers of death in sampled wards, our findings suggest a high asymptomatic spread of the infection and an infection fatality rate of 0·076% in slums and 0·263% in non-slums. ”
All these studies in the Mumbai slums suggest, that in spite of such high statistically significant prevalence of COVID positives, the fatalities have been extremely low.
Source: Seroprevalence of SARS-CoV-2 in slums versus non-slums in Mumbai, India. and Supplementary Data
The World Health Organisation (WHO) Director-General Tedros A. Ghebreyesus, at a press conference on July 10 2020, has lauded the success over the containment of the COVID outbreak in Dharavi (Mumbai slums) —Asia’s largest slum.
“Even in Dharavi, a densely packed area in Mumbai, a strong focus on community engagement and the basics of testing, tracing, isolating and treating all those that are sick is key to breaking the chains of transmission, and suppressing the virus,” Ghebreyesus said.
In this context, the WHO director also pointed out that there are many examples from around the world that have shown that even if the COVID outbreak is very intense, it can still be brought back under control, as in Vietnam, Cambodia, Thailand, New Zealand, Italy, Spain and South Korea.
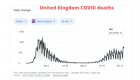
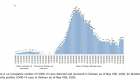
New York: Given these examples one would expect New York’s outbreak to follow a similar pattern. However, the studies show it did not. While New York also practiced lock downs like the Mumbai slums, around the end of March (March 22), it is interesting to note that the deaths not only increased, but they spiked after the lock down.
COVID Lock down in New York
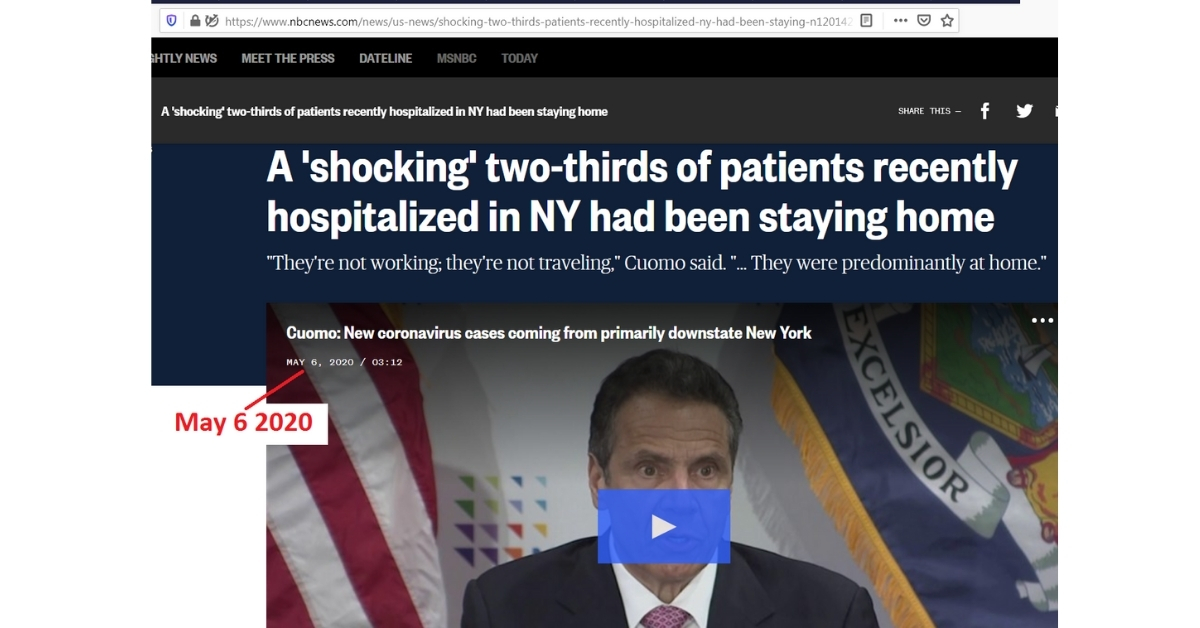
Most new COVID hospitalizations in New York state were from people who were staying home and not venturing much outside, a “shocking” finding, Gov. Andrew Cuomo said in the first week of May 2020.
Surprisingly, early look at the data in May, from 100 New York hospitals, showed that 66% of new admissions related to the virus are people who were at home and the next highest source of admissions was from nursing homes, 18%.
One common response is that may be the slums or homeless populations have more exposure to people with cross-reactive coronaviruses and thus are immune to COVID. It is important to note that prior to this pandemic, nearly 60 – 65 million total visitors visit New York per year (about 50 million domestic and about 13 million international visitors per year). And Mumbai receives 6 to 9 million total visitors per year. So it is very likely that any cross-reactive coronoavirus immunity that possibly provided Mumbai slums from the travelers would have also provided the residents of New York, especially since New York receives comparatively much higher number of international travelers.
For years, New York city has been one of the most visited places, attracting tourists from all over the world. In January 2020 alone, 381,000 passengers arrived from China, according to U.S. Department of Commerce data. During the first half of January, no travelers from China were screened for potential exposure to the virus. Health screening began in mid-January, but only for a number of travelers who had been in Wuhan and only at the airports in Los Angeles, San Francisco and New York. By that time, about 4,000 people had already entered the United States directly from Wuhan, according to VariFlight, an aviation data company based in China. The measures were expanded to all passengers from China two weeks later. Source: NYTimes.
With so much travel to and from New York before the pandemic lockdown, New Yorkers are extremely likely to have been exposed to cross-reactive coronaviruses from across the world even before the March 22 lockdown. In other words, cross-reactive coronavirus exposure and consequent immunity against the family of coronaviruses is unlikely the only significant reason for immunity exclusive to the people of Mumbai slums. Further tests need to be conducted to see the levels of cross-reactive T cells along with antigen and antibody titers from samples before (if available) and after the COVID outbreak both in the Mumbai slums and New York.
While we need more scientific data, some reports have also claimed that the deaths in the Los Angeles homeless population appears to be lower than expected, again potentially contradicting what one would expect. It is important to note that the homeless are eligible to receive medicaid treatment in hospitals for COVID and the recorded deaths are from hospital files. That is why it is important to distinguish between homeless COVID deaths who died in the hospitals vs homeless COVID deaths who died outside the hospitals. I will expand more on homeless deaths in the future as I get more information. LATimes low homeless deaths.
Thus, there seems to be a disproportionately high number of deaths in areas with better hospital facilities like rich neighborhoods in New York compared to poorer, underdeveloped, underfunded hospital areas such as Mumbai slums where ventilators and other oxygen equipment are not readily available. A similar pattern is also seen in a study in the slums of Dhaka, Bangladesh with high prevalence of infection and a very low death toll. By July 2020 in Dhaka city, Bangladesh, the seroprevalence of COVID antibodies was 45% while in the slums of Dhaka it was 74% with a very low death toll.
Source: NYTimes: Why has Covid’s toll been surprisingly low across much of Africa and Asia?
This appears to be a complete paradox – one would expect places with well funded hospitals and better access to equipment like ventilators to have lower deaths than places with access to less-advanced healthcare systems.
Different hypotheses have been proposed for the low death toll in the Mumbai slums (and also in Asia and Africa in general).
Some of them are as follows:
Alternate Hypothesis 1: “Poorer countries are younger: COVID is usually harder on older people: More than 80 percent of U.S. deaths have occurred among people who are 65 or older. Nursing homes — where COVID has often spread from one resident to the next — are more common in Western countries. Outside the West, older people often live in multi-generational households.”
Argument against this hypothesis: The Mumbai slums study in The Lancet journal, showed that in individuals 60 years and older, the proportions of positive tests were not only high, it was in fact significantly higher when compared to 25–39 years old individuals (p<0·001). In other words by the end of July 2020, a high proportion of the older population in the slums were not only already exposed to COVID and expressing COVID specific antibodies, but also survived with a low fatality rate. The data from the Mumbai slum studies also suggests, that individuals in slums live in multi-generational households with a high proportion of younger population, which did not decrease the exposure of the older slum population to COVID, in fact, it turned out they survived in-spite of the high exposure (antibody positive).
Source: Seroprevalence of SARS-CoV-2 in slums versus non-slums in Mumbai, India.
Alternate Hypothesis 2: “Fresh air helps: Daily life tends to be better ventilated in warmer, lower-income countries. People spend more time outdoors, and windows are often open. COVID spreads less easily in these settings than it does in poorly ventilated indoor spaces.”
Argument against this hypothesis: As shown from the sources and images in previous paragraphs, 57% of the people in slums share 1 room huts, and many live in hutments sized 10 feet x 10 feet with hardly any ventilation. This in no way can be described as having better ventilatory conditions when compared to the western homes and nursing homes.
Alternate Hypothesis 3: “Immunity may not be uniform: Did prior exposure to other coronaviruses including those that cause the common cold provide a degree of resistance? If previous coronaviruses spread more widely in some countries, then people’s immune systems there may be better prepared to fight COVID. Some researchers have argued that deaths are lower in countries which have a higher population exposed to a diverse range of microbes.”
Argument against this hypothesis: The Mumbai slums studies show that by the end of July 2020, a large proportion of the slum population had developed COVID specific antibodies (54.1% in one study and 57% in another) and survived, suggesting that the survival protection to COVID was mainly due to COVID specific antibodies irrespective of other non-specific coronavirus and common cold virus antibodies. Furthermore, the potential exposure to other non specific coronaviruses is likely higher in places of high international travel such as New York compared to the Mumbai slums as described above in detail.
Alternate Hypothesis 4: “Policy matters: Countries have restricted entry at their borders, many countries did lock-downs, rapid COVID tests and quarantines.”
Argument against this hypothesis: Over 30 scientific studies suggest lock-downs probably did not control the virus. Sources: Lockdowns Do Not Control the Coronavirus: The Evidence.
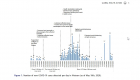
On November 26 2020, India witnessed the largest organized strike in human history. Over 250 million workers and farmers, along with their allies among student, women’s, and civil society groups, participated in a nationwide strike for several days. Although social distancing and mask regulations were barely followed at most of the places where this massive strike was conducted, the number of deaths did not increase proportionately. During the same period the deaths in the US and the UK increased at a much higher rate than in India as can be seen from the Johns Hopkins COVID death data in the slideshow below. Note that the United States population is 331+ million people, United Kingdom population is 68+ million people and the population that actually participated in the strike in India was close to 250 million.
The largest general strike in the world (250 million people) happened in India in the middle of the pandemic in late November 2020 but the number of deaths did not increase proportionately
Several countries with much less-advanced healthcare systems have emerged successful in responding to COVID
Vietnam
Vietnam, a country of 97+ million people, despite its long border with China and millions of Chinese visitors it receives each year has extremely low number of deaths (35 deaths as of December 2020). This is all the more remarkable considering Vietnam is a low-middle income country with a much less-advanced healthcare system than others in the region. It only has 8 doctors for every 10,000 people, a third of the ratio in South Korea, according to the World Bank. After a nationwide lockdown, Vietnam lifted some social distancing rules in late April. Businesses and schools have reopened, and life is gradually returning to normal. Researchers attribute Vietnam’s success in controlling COVID to widespread testing, quarantine of potentially exposed persons, and rapid contact tracing. Vietnam also recently reopened its borders to international travelers. Source: Lessons learned from Vietnam’s COVID-19 response: the role of adaptive behavior change and testing in epidemic control.
In this context, one of the discussions often brought up is herd immunity. According to Johns Hopkins Bloomberg School of Public Health – “When most of a population is immune to an infectious disease, this provides indirect protection—or herd immunity (also called herd protection)—to those who are not immune to the disease. For example, if 80% of a population is immune to a virus, four out of every five people who encounter someone with the disease won’t get sick (and won’t spread the disease any further). In this way, the spread of infectious diseases is kept under control. Depending how contagious an infection is, usually 50% to 90% of a population needs immunity to achieve herd immunity.”
It is important to note for example that if a hypothetical elder person happens to be susceptible to severe COVID infection in February 2020, he or she will continue to be susceptible in December 2020 (assuming the persons’ health condition remains the same) irrespective of herd immunity (there are some exceptions such as if the virus mutates and is dominated by a milder form, or a vaccine etc). Social distancing and mask regulations just delays the potential exposure of the person to the virus. In other words, a reversal of lockdown should see a spike of deaths along with increase in positive cases in those areas. In this context it is also important to note that there were tens of thousands of elderly population (susceptible population) in both the Mumbai slums as well as the November/December 2020 general strike in India and yet the number of deaths were relatively low compared to parts of the world with better hospitals.
Some experts also agree depending on herd immunity is a dangerous strategy. Sources: COVID-19 Story Tip: Herd Immunity Is a Dangerous Strategy for Fighting COVID-19, Says Johns Hopkins Expert and Early Herd Immunity against COVID-19: A Dangerous Misconception.
2. Almost all COVID deaths recorded were on some form of ventilatory support.
Summary:
- Almost all COVID deaths that have been reported were on some form of ventilatory support – Positive Pressure Ventilation, Supplementary Oxygen etc.
- It is interesting to note that parts of the world with less advanced ventilatory support facilities compared to USA and UK, happen to show lesser number of COVID deaths. Examples: Grenada, Antigua and Barbuda, Barbados, Papua New Guinea, Taiwan, Mauritius, Tanzania, Botswana, Maldives, Vietnam, Cuba, Malta, Guyana, Namibia, Nicaragua, Bahamas, Mali, Belize, Mauritania, Malawi, Uganda, Haiti etc.
- While the low number of deaths can possibly be accounted to lockdowns in these countries, it does not account for the lack of deaths (as of December 2020) after the reversal of lock-down, because the spread of COVID is only delayed with the lock-downs not contained. Source of deaths: https://coronavirus.jhu.edu/data/mortality
Almost all of the reported COVID deaths throughout the world, throughout 2020 were on some form of ventilatory support including the published data from Wuhan, China.
Were the COVID patients who died put on ventilatory support because they were close to terminal stages or did they reach terminal stages due to the downsides of ventilatory support?
Are COVID patients more susceptible to pulmonary injury by ventilatory intervention compared to most other viral, bacterial or fungal infections?
It is interesting to note that while the number of positive cases have increased with the reversal of lock downs in many countries (by December 2020) the number of non-hospitalized (and non-ventilatory supported) deaths have not increased in many of the poorer countries. In fact there are extremely low number of COVID deaths who were not hospitalized and not on any form of ventilatory support or oxygen therapy thoughout the year 2020. If our hypothesis is false, we should be seeing a flood of COVID deaths, along with the increased number of COVID positives in remote poorer parts of the world where there is shortage or limited access to ventilatory support (such as Mumbai slums, people of islands with limited ventilatory support and who have restricted air travel access to fly to advanced hospital facilities). However, thus far we have seen the opposite.
3. Understanding the complexities associated with mechanical ventilation and oxygen therapy.
Summary:
- Mechanical ventilation and supplemental oxygen are lifesaving interventions and have impacted millions of lives since their invention, but they are not without complications. Some common conditions that can be associated with ventilator-associated events are pneumonia, atelectasis, fluid overload and acute respiratory distress syndrome, some of which are similar to the autopsies of COVID deaths. Source: Potential Strategies to Prevent Ventilator-associated Events and 18 COVID autopsies. Studies show that the indications and guidelines of correct timing for the initiation, maintenance and termination of ventilatory support are constantly changing with ongoing research. Added to this are the challenges in updating and monitoring these guidelines.
- Similarly, Oxygen therapy has life-saving potential, however, excessive oxygenation and oxygen given without appropriate assessment and ongoing evaluation can lead to oxygen toxicity manifested as system wide cellular injury, airway injury and lung parenchymal injury due to reactive oxygen species, barotrauma and alveolar damage among other reasons.
- Lapses of understanding and communication among the physicians, nurses, and respiratory care practitioners managing the ventilated patient, can adversely affect morbidity, and ultimate outcome. The British Thoracic Society guidelines study and other studies elaborated below show the difficulties in training, monitoring and implementing the latest ventilatory guidelines to patients. Source: Complications associated with mechanical ventilation. More sources below.
a. Benefits of mechanical ventilation and supplemental oxygen therapy.
There are numerous studies showing the benefits of mechanical ventilation and oxygen therapy. Below slideshow is a small list of studies published demonstrating the benefits of mechanical ventilation and oxygen therapy:
b. Complications and difficulties of mechanical ventilation and supplemental oxygen therapy.
Oxygen can be vital during critical illness. Studies show hypoxia (low tissue oxygenation) is an indication to start oxygen therapy; this can be a life-saving intervention, but given without appropriate assessment and ongoing evaluation, it can also be detrimental to patients’ health (Ridler et al, 2014) and hyperoxia (excess oxygen) may in fact harm patients. Source: Oxygen therapy in critical illness: friend or foe? A review of oxygen therapy in selected acute illnesses.
Societies such as British Thoracic Society, Thoracic Society of Australia and New Zealand, American Thoracic Society etc regularly publish guidelines for the use of oxygen therapy and mechanical ventilation.
In this section, I will be analyzing some of the published guidelines, recommendations and the deficiencies in our knowledge about the use of oxygen therapy and mechanical ventilation.
For more information about ventilatory therapy and the basics of oxygen therapy the sources are linked below and here: Arterial Blood Gas analysis
“It is worrying that the few existing trials of oxygen therapy given to non-hypoxaemic patients in common conditions such as heart attacks, strokes and difficult labour have failed to show benefit, and there have been suggestions of possible harm in these trials despite the near universal use of oxygen for such conditions in the past.” Source: BTS guideline for emergency oxygen use in adult patients.
The British Thoracic Society oxygen audit in 2015 involving 55K+ patients (one of the largest studies of oxygen audit), demonstrated areas of poor practice for oxygen prescribing, administration, and monitoring in that:
- Forty-three percent of patients on oxygen had no valid prescription for it.
- Only 53% had a target SpO2 range prescribed despite 70% of audited hospitals having a policy requiring a range to be set (SpO2 is arterial oxygen saturation measured via pulse oximetry; abbreviations at the end of this article).
- Sixty-nine percent of patients with a range prescribed had SpO2 values within the required range; 9% had SpO2 values below and 22% above.
- Nine percent of patients receiving oxygen were identified as being at risk of type 2 respiratory failure because SpO2 values exceeded their target.
“If referring to any other prescribed drug these results would be totally unacceptable, for example on any given day 6000 patients were receiving oxygen without any written order. Perhaps it is still widely assumed that using oxygen in the acutely ill patient cannot be harmful despite the growing body of evidence suggesting otherwise.”
Source: Hyperoxia in anaesthesia and intensive care.
A systematic review and meta-analysis of 19 cohort studies concluded hyperoxaemia was associated with increased in-hospital mortality in critically ill patients, but caution was advised again in the interpretation of the results because of the heterogeneity of studies included. Source: Association between arterial hyperoxia and outcome insubsets of critical illness: a systematic review, meta-analysis, and meta-regression of cohort studies.
A 2017 large (14, 441 patients) observational study again found a U-shaped relationship between mean PaO2 whilst in the ICU and mortality, with both the degree and duration of hyperoxia adversely affecting outcome. Source: Metrics of Arterial Hyperoxia and Associated Outcomes in Critical Care.
A study in Critical Care in 2018, concluded that emergency department exposure to hyperoxia is common and associated with increased mortality in mechanically ventilated patients achieving normoxia after admission. This suggests that hyperoxia in the immediate post-intubation period could be particularly injurious, and targeting normoxia from initiation of mechanical ventilation may improve outcome. Source: Emergency department hyperoxia is associated with increased mortality in mechanically ventilated patients: a cohort study.
It had been known for several decades that oxygen can be a life-saving drug for patients with severe hypoxaemia but excessive amounts of oxygen can be harmful, especially for patients with exacerbated chronic obstructive pulmonary disease (COPD) and those with other conditions which make them vulnerable to hypercapnic respiratory failure. In addition, it has not been shown to have any effect on the sensation of breathlessness in non-hypoxaemic patients.
“Although medical oxygen is a drug, local audits in several countries have shown that there are significant problems with the use of oxygen in hospitals and in ambulances. These surveys have reported that oxygen was commonly used without any prescription and prescriptions, if they did exist, were rarely followed at the bedside. The British Thoracic Society guideline for emergency oxygen use in adult patients was commissioned by the British Thoracic Society and developed in conjunction with 21 other colleges and societies.” Source: British Thoracic Society emergency oxygen audits.
According to British Thoracic Society emergency oxygen audits, oxygen prescribing and administration in the UK was highly unsatisfactory prior to the publication of the British Thoracic Society guideline in 2008 and is improving slowly. An audit in 2009 and 2010 in the UK showed continued struggles in implementing and monitoring the oxygen policies.
Close monitoring of hypoxemia is essential. At the same time unnecessary use of oxygen can cause harm rather than benefit as recommended in the British Thoracic Society guidelines below:
Source: BTS guideline for oxygen use in adults in healthcare and emergency settings.
Oxygen is probably the commonest drug to be used in the care of patients who present with medical emergencies. Currently, ambulance teams and emergency department teams are likely to give oxygen to virtually all breathless patients and to a large number of patients with other conditions such as ischaemic heart disease, sepsis or trauma. For example, the North West Ambulance Service serves a population of about 7.25 million people in the U.K. and transports about 700,000 people to hospital emergency departments each year. About 34% of these journeys involve oxygen use at some stage: Source. This translates to about two million instances of emergency oxygen use per annum by all UK ambulance services, with further use in patients’ homes, general practice surgeries and in hospitals.
At present, oxygen is administered for three main indications of which only one is evidence-based. First, oxygen is given to correct hypoxaemia as there is good evidence that severe hypoxaemia is harmful. Second, oxygen is administered to ill patients in case they might become hypoxaemic. Recent evidence suggests that this practice may actually place patients at increased risk if severe hypoxaemia does actually develop. Third, a very high proportion of medical oxygen is administered because most clinicians believe that oxygen can alleviate breathlessness. However, there is no evidence that oxygen relieves breathlessness in non-hypoxaemic patients and there is evidence of lack of effectiveness in non-hypoxaemic breathless patients with chronic obstructive pulmonary disease (COPD) and advanced cancer.
One small double blind trial reported that hypoxaemic patients with advanced cancer (SpO2, 90%) had reduced dyspnoea breathing oxygen compared with air, but a larger and more recent study failed to show benefit from oxygen compared with air, even when hypoxaemia was present.
Sources:
– A randomized, double-blind, crossover trial of theeffect of oxygen on dyspnea in patients with advanced cancer.
– Effects of oxygen on dyspnoea in hypoxaemic terminal-cancer patients.
“Unfortunately, many clinical studies have shown that patients with COPD are frequently given very high doses of oxygen, either because of misdiagnosis or because the risks of hyperoxia in patients with COPD have been overlooked. Also many patients with COPD are unaware of the diagnosis or are mislabelled as having asthma.”
Sources:
– One year period prevalence study of respiratory acidosis in acute exacerbations of COPD: implications for the provision of non-invasive ventilation and oxygen administration.
– The effects of oxygen therapy in patients presenting to an emergency department with exacerbation of chronic obstructive pulmonary disease.
– The use of oxygen in acute exacerbations of chronic obstructive pulmonary disease: a prospective audit of pre-hospital and hospital emergency management.
– Acute hypercapnic respiratory failure inpatients with chronic obstructive lung disease: risk factors and use of guidelines for management.
– BTS guideline for emergency oxygen use in adult patients.
Most of the Thoracic Society’s recommendations are classified based on the robustness of the available evidence and are given hierarchy in the level of confidence for the treatments as shown in the slideshow below. For example, some treatment recommendations are “Grade D” evidence which is based on “expert opinion or case reports” due to lack of trials, which shows the deficiencies in our knowledge regarding oxygen therapy and mechanical ventilation. To quote British Thoracic Society: “It is worrying that the few existing trials of oxygen therapy given to non-hypoxaemic patients in common conditions such as heart attacks, strokes and difficult labour have failed to show benefit, and there have been suggestions of possible harm in these trials despite the near universal use of oxygen for such conditions in the past“.
One 2018 study concluded that many deficiencies were observed regarding the nasal oxygen practice in ICUs and lagged behind the guideline recommendations in some hospitals in China.
Pulse oximetry is ubiquitously used for monitoring oxygenation in the critical care setting and is one of the crucial steps in making critical decision about introducing ventilatory support. By forewarning the clinicians about the presence of hypoxemia, pulse oximeters may lead to a quicker treatment of serious hypoxemia and possibly circumvent serious complications. However, pulse oximetry is not without limitations. Because of the sigmoid shape of the oxyhemoglobin dissociation curve, oximetry may not detect hypoxemia in patients with high arterial oxygen tension (PaO2) levels. Sources: Pulse oximetry and Potential errors in pulse oximetry. I. Pulse oximeter evaluation. In addition, the struggles of catching up to the constantly changing guidelines in learning, monitoring and implementing pulse oximetry among clinicians appear to be limited.
Although pulse oximetry (SpO2) readings can correlate with one-point measurements of SaO2, studies showed that it did not reliably predict equivalent changes in SaO2, particularly in intensive care unit patients. Sources: Accuracy of pulse oximetry in the intensive care unit and Do changes in pulse oximeter oxygen saturation predict equivalent changes in arterial oxygen saturation?
While home oxygenation kits can be convenient, the lack of knowledge and monitoring at home makes it risky. While we do not know the exact cause of death, there is at-least one instance of a news article of a person who died and happens to have self medicated himself with oxygen mask at home after he contracted COVID. Source: Russian influencer died of COVID.
c. Understanding the complexities in ventilatory and oxygen support.
Ventilatory medicine is still an evolving subject with added complexities, and medical professionals need constant updates.
For those interested here is a good course to understand some of the current basics of ventilatory support:
Definition of terms:
- FiO2: Fraction of inspired oxygen (%).
- PaCO2: The partial pressure of CO2 in arterial blood. It is used to assess the adequacy of ventilation.
- PaO2: The partial pressure of oxygen in arterial blood. It is used to assess the adequacy of oxygenation.
- SaO2: Arterial oxygen saturation measured from blood specimen.
- SpO2: Arterial oxygen saturation measured via pulse oximetry.
- Heat Moisture Exchange (HME) product: are devices that retain heat and moisture minimizing moisture loss to the patient airway.
- High flow: High flow systems are specific devices that deliver the patient’s entire ventilatory demand, meeting, or exceeding the patients Peak Inspiratory Flow Rate (PIFR), thereby providing an accurate FiO2. Where the total flow delivered to the patient meets or exceeds their Peak Inspiratory Flow Rate the FiO2 delivered to the patient will be accurate. High flow in approved areas only. Consult your NUM if unsure.
- Humidification is the addition of heat and moisture to a gas. The amount of water vapour that a gas can carry increases with temperature.
- Hypercapnea: Increased amounts of carbon dioxide in the blood.
- Hypoxaemia: Low arterial oxygen tension (in the blood.)
- Hypoxia: Low oxygen level at the tissues.
- Low flow: Low flow systems are specific devices that do not provide the patient’s entire ventilatory requirements, room air is entrained with the oxygen, diluting the FiO2.
- Minute ventilation: The total amount of gas moving into and out of the lungs per minute. The minute ventilation (volume) is calculated by multiplying the tidal volume by the respiration rate, measured in litres per minute.
- Peak Inspiratory Flow Rate (PIFR): The fastest flow rate of air during inspiration, measured in litres per second.
- Tidal Volume: The amount of gas that moves in, and out, of the lungs with each breath, measured in millilitres (6-10 ml/kg).
- Ventilation – Perfusion (VQ) mismatch: An imbalance between alveolar ventilation and pulmonary capillary blood flow.
-
Ventilation: Exchange of air between the lungs and the air (ambient or delivered by a ventilator), in other words, it is the process of moving air in and out of the lungs. Its most important effect is the removal of carbon dioxide (CO2) from the body, not on increasing blood oxygen content. Ventilation is measured as minute ventilation in the clinical setting, and it is calculated as respiratory rate (RR) times tidal volume (Vt). In a mechanically ventilated patient, the CO2 content of the blood can be modified by changing the tidal volume or the respiratory rate.
-
Oxygenation: Interventions that provide greater oxygen supply to the lungs, thus the circulation. In a mechanically ventilated patient, this can be achieved by increasing the fraction of inspired oxygen (FiO 2%) or the positive end-expiratory pressure (PEEP).
-
PEEP: The positive pressure that will remain in the airways at the end of the respiratory cycle (end of exhalation) that is greater than the atmospheric pressure in mechanically ventilated patients. For a full description of the use of PEEP, please review the article titled “Positive End-Expiratory Pressure (PEEP).”
-
Tidal volume: Volume of air moved in and outside the lungs in each respiratory cycle.
-
FiO2: Percentage of oxygen in the air mixture that is delivered to the patient.
-
Flow: Speed in liters per minute at which the ventilator delivers breaths.
-
Compliance: Change in volume divided by change in pressure. In respiratory physiology, total compliance is a mix of lung and chest wall compliance as this two factors cannot be separated in a live patient.
Source: Ventilator Management and Oxygen delivery.
To be continued…